Lifespan.io: Cyclarity Launches Human Trial to Cure Atherosclerosis
By Steve Hill at Lifespan.io
Recently, Cyclarity Therapeutics announced the launch of a Phase 1 human clinical trial for a drug that aims to remove the arterial plaques that lead to heart attacks and strokes.
Tackling the leading cause of death worldwide
Cyclarity Therapeutics is working on a cost-effective small molecule drug aimed at eliminating arterial plaque, thus potentially addressing the globally leading cause of death: cardiovascular disease.
Its primary cyclodextrin drug candidate, UDP-003, focuses on 7-ketocholesterol, a type of oxidized cholesterol that increases in cells and tissues as people age. Atherosclerosis occurs when plaque accumulates in the arteries, primarily due to this oxidized cholesterol buildup.
This clinical trial will take place at CMAX, a leading clinical research center in Australia, in partnership with Monash University. As the clinical trial is set to start this year, we feel that this is the right moment to connect with Dr. Matthew O’Connor from Cyclarity to learn more about this important advancement.
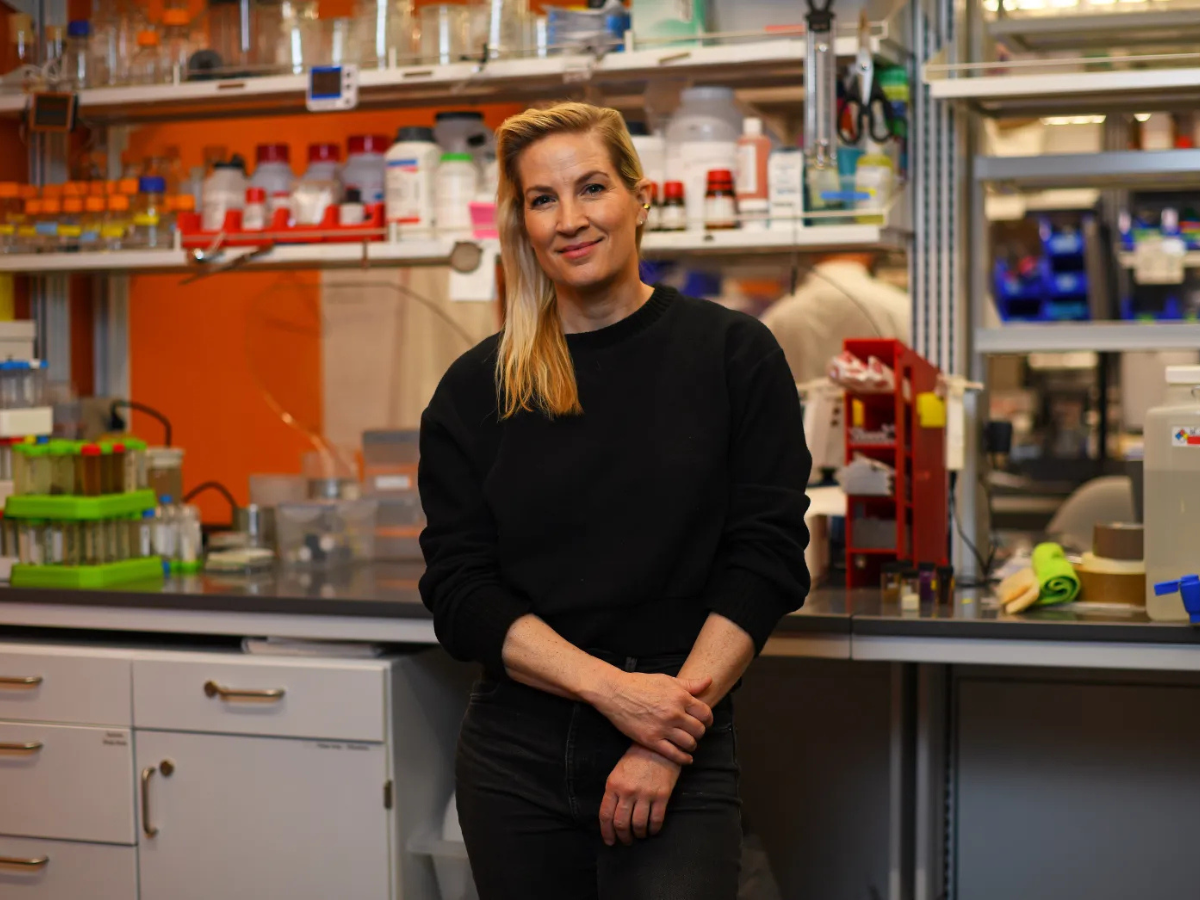
Dr. Matthew O’Connor formerly worked for the SENS Research Foundation, which merged with Lifespan.io last year to establish the Lifespan Research Institute, where the initial concepts for Cyclarity originated. He now holds the position of CEO of Scientific Affairs at Cyclarity.
Hi Matthew, and thanks for joining us for this interview. So, first off, congratulations on reaching this important milestone, it has been quite a while coming. How do you feel about Cyclarity finally achieving this goal?
It’s really a dream come true. For me, or any researcher really, to get something that we developed and worked on over the course of years to this point is great. First, it’s just an idea, then you do some proof-of-concept research, then you put a lot of blood, sweat and tears into it over the course of years. And then to have something that you worked on from the beginning coming all the way to people, and you get to find out if it can actually help people, it’s a dream come true. It’s an amazing feeling.
I can imagine, it’s really quite an achievement, and we’re all very excited about it. Before we dive into things, could you briefly explain how UDP-003 works to remove plaques?
So, what we’re trying to do is convince your own immune cells, in particular a type of immune cell called the macrophage, to go and eat up the plaque. In fact, that’s what the macrophage already wants and tries to do.
But, when it comes to the buildup of plaques, when the macrophage tries to eat them, it absorbs too much oxidized cholesterol (7-ketocholesterol) from inside them. It cannot metabolize the oxidized cholesterol, so it shuts down and balloons in size, becoming a nasty kind of cell called a foam cell.
Foam cells are just big bloated cells that sit there and contribute to the problem of the plaque rather than resolving it like the macrophage is supposed to do. So, what our treatment does is turns the foam cell back into a healthy macrophage and allows it to go back to doing its job. Our drug specifically binds this oxidized cholesterol form, pulls it out of the plaques and macrophages, and just floats away with it to be excreted. That allows the plaque to shrink and the artery wall to heal.
Also, there is a myth about our drug that it works like Drano and is just going to wash away your plaque. It’s not quite that simplistic, and that might be dangerous. What our drug targets is the small amount of oxidized cholesterol that’s in your plaque and then allows it to resolve and heal on its own over the course of a few months after the treatment.
Well, that would be amazing. And we’ve talked about this in our last interview, that it has the potential to help 70 to 80 percent of people who are at risk of heart attacks and or strokes. It would be wonderful to have a real solution to the number one cause of death in the world. I would think that with the Phase 1 that you’re about to start, you’re probably already fully enrolled with participants?
No, not yet.
Well then, how might people go about enrolling if they’re interested?
The enrollment will officially open on or around January 22nd. We’re not managing the trial directly; there’s a professional trial site and company that’s managing it, but we will put up the volunteer information on the Cyclarity website and the Cyclarity Facebook page as soon as that information is available.
That sounds fantastic, and needless to say, I think you’re going to be inundated. Now onto a question I asked you when we did the previous Cyclarity interview last February. It’s been almost a year since we last talked, and based on your experiences since then, what has been the greatest challenge getting UDP-003 into the clinic?
Overall, it’s about creating a product that you’ve tested is safe in every way you can before moving it to people: that you have the drug product manufactured correctly, properly, and well documented. The amount of work and documentation that goes into that process is simply harrowing.
I won’t bore you or your audience with all of the nitty-gritty details, but it’s an enormous amount of work, and we’ve gone through every step of the process and the review committee in Australia.
We’ve also talked to regulators in the UK and in the US to get international feedback to make sure that what we’re doing in Australia is going to be transferable to an international realm. It’s a lot of work to get from something that’s working in a test tube in the lab to being ready to start dosing people.
Yeah, it is a tremendously long journey. You’ve got the in vitro and the animal testing stages before something can even get anywhere near people. So it’s an amazing achievement that you have reached this point.
But anyway, as most conversations eventually turn to, let’s talk about money. Cyclarity has just closed the first tranche of a Series A funding round, which was somewhere around about 6.4 million US dollars. Could you tell us a little bit more about how these funds will be used?
Yes, of course, and I’ll just clarify one thing, which was that it was actually the first part of a series A funding round, and the second part is still open. We’re hoping to close on that in the next month or two. We actually still need to raise the rest of the round in order to complete the entirety of the Phase 1 trial that has been approved by the regulators.
What this 6.4 million will pay for, in terms of the clinical trial, is the safety-only part in healthy volunteers. So, there’ll be 72 healthy volunteers, half of whom will get a single dose of our drug and half of whom will get six doses.
The second part, the multiple dosing program, is what the eventual design of the dosing regimen is planned to be, and that’s what will get used in the second part of Phase 1.. We still need to raise at least another $2.6 million to be able to pay for it.
Raising money is hard to do, and we are always raising money, and there’s not any end to that in sight.
Yes, there’s few things as expensive as research, especially medical research. I definitely sympathize, so hopefully there are some people reading this who have the means and might be interested in putting funds into it.
So let’s talk a little bit about the personalities driving this trial. You’ve opted to work with Dr. Stephen Nicholls, the director of the Monash Victorian Heart Institute in Melbourne, and he’s also a professor of cardiology at Monash University. What made you decide to work with him, and how has your experience been with him so far?
We’re really lucky to get to work with Professor Nichols on this project and to get his advice and feedback on our clinical strategy and on the trial to have him leading the effort. It was really thanks to him that we ended up deciding to do our initial clinical trials, and hopefully later phases of the clinical trials, in Australia.
Really, he’s just an amazing guy to work with. He has a phenomenal history, he came out of cardiology at the Cleveland Clinic in the U. S., and he’s the type of person that the big pharmaceutical companies call to oversee their end-stage clinical trials for cardiovascular drugs that are out there now.
He’s been associated with some of the statins and now the other lipid-lowering drugs that he’s working on. To have somebody like him be excited about our drug and the potential that it has to reverse plaque rather than just slowing down the accumulation, which is what the lipid-lowering drugs do, is just amazing.
He’s been really generous with his advice and his time, and he has an amazing team of people to help make all these things happen. That’s really a lot of the value that he bought, introducing us to people who work at Monash University, who can advise us at the Victorian Heart Institute, and at CMAX where we are running the trial. There’s so many people that he has around him who help make magic happen in the cardiovascular field. It’s a real privilege to work with him.
Yes, he is quite a well-known personality in the medical world. He sounds like the perfect choice. Circling back, you mentioned big pharma just now, has there been much interest from Big Pharma in UDP-003? Or are they just watching from the sidelines waiting to see what happens?
We’ve had a number of productive discussions with pharmaceutical companies, and we anticipate wanting to partner with a large pharmaceutical company later on, especially in a large disease indication space like cardiovascular disease.
Atherosclerosis, broadly speaking, is not a tiny niche group of rare disease patients where you might be able to run that with a small biotech company on your own. It’s really something that requires a lot of international infrastructure that the big partners can bring to the table.
So, we’ve had a lot of good discussions. I’d say the summary of the situation is that they want to see the results. They’re excited about the fact that we’ve gotten into the clinic and they want to see the results of Phase 1. They want to see the safety, the blood work, the urine test results and see if the drug is doing, at least at the molecular level, what we claim it’s supposed to do.
Yeah, so they are hedging their bets at the moment, but they’re definitely interested, which is good because we’re going to need big pharma with any of these interventions our field is working on. Of course, we talked about the scalability of the technology last time we spoke, and it does have potential to be produced at scale, which is where Big Pharma comes in.
This is a question that relates to the road that you’ve traveled to get to this point, because you were originally looking at working in doing it in the US via the FDA. Then, you were exploring working with the NHS in the UK but that didn’t pan out, and you finally moved to start up in Australia. So, how does the Australian healthcare system differ from the U.S. and the U. K. in the context of launching trials?
The biggest difference is that it’s somewhat more decentralized than in most countries. In our case, we are working with a Human Research Ethics Committee (HREC) that has national jurisdiction but is one of a number of HRECs in the Australian system. The effect of doing things like this is that it makes for a more decentralized system that has a lower level of bureaucracy.
The other thing, at least with the FDA, is that you’re expected to file your clinical trial application and get it right the first time, and so you put an enormous amount of work into guessing what they could possibly want to see. They will still come back with questions, but there’s a very tight timeline. If you fail to meet it, you get put on clinical hold, which makes your company look very bad, and you have to start over with the application process.
But, in Australia, the way it works is you submit an application, and it’s not expected to be perfect on the first try. You just submit something that is a little bit briefer than what you would do in some other countries and a little less detailed. Then, you wait for their feedback and their questions and see what they want more information about, what concerns they have, and what feedback they have about your clinical trial protocol.
Then, you respond to their questions, and they look at your responses. They can then respond with more questions, and that back and forth can happen however many times it takes. So, it’s a bit more of an iterative process, which I think makes it just as thorough as the other countries, but it’s a bit more nimble and efficient and designed to get therapies into the testing phase as efficiently as possible.
So, speaking a bit more about the Australian healthcare system. The approach that our field embraces is directly targeting the biology of aging, and UDP-003 is very much targeting one of those processes to prevent disease. In the past, there has been significant pushback against this idea from the medical community. Does the one disease at a time approach, what I call whack-a-mole, still pervade?
From that perspective, the Australian policies and the agencies in Australia are pretty similar to other countries.
They’re focused on disease indications and outcomes measures in that way, so we have described our drug in those terms rather than as an anti-aging drug or something like that. Fortunately, since science is logical, if you’re targeting a fundamental aspect of aging, it should be possible to connect the dots and explain why it’s going to help this disease or that disease.
So, in that respect, it hasn’t been any different than you would expect to see in any other country, and we haven’t tried to sell the regulators on the idea that our drug is an anti-aging drug. But, there’s certainly wide recognition that with chronic diseases like atherosclerosis, the main risk factor is a person’s age, and that’s the target of our drug.
They’re happy to acknowledge a new target for a specific disease indication, and as long as you can explain the logic of it and show some evidence, then they can give you a shot. So in that respect it’s not really any different from any other country.
Yes, that makes sense, and at the end of the day if it’s demonstrated to work through the established systems, then it works. Next, I’d like to take you back in time. You worked at the SENS Research Foundation, which merged last year with Lifespan.io to form the Lifespan Research Institute (LRI), for nine years. Can you tell me about your early research experience there and how did it help you move towards launching Cyclarity?
When I first joined the SENS Research Foundation in 2010 I was initially hired to work on mitochondrial aging and to develop a mitochondrial gene therapy to help resolve the mutations in mitochondrial DNA that accumulate with age. That was a great project, and we did a lot of good research. It was challenging but also fruitful and we built a good team and published some nice papers, and that work is ongoing by Dr. Amutha Boominathan and her team at the LRI.
But not too long after being at the institute, I got involved in helping to manage all of the research that we were doing at our research center in Mountain View, California, and research that we were funding around the world focused on damage repair. These were types of projects either characterizing the damage or looking at ways to resolve the kinds of damage that we had identified.
So it was that step of getting exposure to all the different kinds of research that we were doing that led to me taking a project that was being done at a university externally and bringing the project into our research center. Next, we completely changed it into a different approach from what had been done previously by the academics.
This led to us making the discoveries that we made, to being able to write patents, and eventually form a company and spin it out of the foundation bringing some of the team with us. That’s how that all came together through the SENS Research Foundation.
It’s great to see that nonprofits have an important role in getting these things off the ground, and obviously in your case, it’s definitely succeeded, and here we are at this very important moment. I think it’s fair to say that if you guys do succeed, it would be pretty strong validation for the idea that the damage repair approach towards aging and age related diseases is viable.
So, now for the big question and what most readers will be wanting to know. With the caveats that clinical trials have at least three phases and this takes time and assuming everything goes to plan and the data is good, when might this therapy become available?
With the traditional system of doing Phase 1, 2, 3, and then being approved for market, the fastest route would be by 2030. That would be about the quickest time that I could imagine full approval under the current system.
That said, we’re really interested in some of the accelerated and adaptive approaches that are being developed. For example, we received the Innovative Licensing and Access Pathway award (ILAP), in the UK, which allows for partial reimbursement by the UK healthcare system in late-stage clinical trials.
If it looks like the drug is working as promised, if it seems likely that it’s working, if it appears that it’s helping people, then we may be able to start gradually releasing it in places like the UK that may start allowing this. Rather than this sort of all-or-nothing system that most of the world uses now, where it either hasn’t been completely proven to be safe and effective, or it’s been completely proven to be safe and effective.
Right now, the overwhelming practice is that you have to prove beyond any shadow of a doubt that it’s safe and effective. Then, it gets fully released and anyone with the approved diagnosis can receive the treatment. That’s pretty black and white, and I think there’s more gradual approaches that hopefully will be available to us soon in the UK and other places. And who knows, maybe in the US, they’ll start experimenting with systems like that as well.
There’s a lot of innovation in clinical trials that are being experimented with in different places right now that we’re paying close attention to and looking for opportunities to try to bring our therapy to people as soon as it’s ready.
It strikes me that systems like RMAT in the USA may be a possible avenue as well. That’s a framework that’s attempting to get with the times and accommodate approaches like gene therapies, regenerative medicine and the new technology that’s coming. As you say, there could be other systems in development that may allow us to accelerate its distribution globally a little bit faster. Also, existing data in one area may also mean you’re not having to start a Phase 1 in every single country.
The last question I’ve got for you is: what’s next for the Cyclarity team?
Of course, we’re mostly focused on developing our lead drug for atherosclerosis, but there’s other related indications that we’re also exploring. So, atherosclerosis and the associated dyslipidemias could be caused by oxidized cholesterol accumulation, where we’re closely investigating the impact on brain aging, and oxidized cholesterol is strongly implicated. We have also got a grant to study our drug in relation to Alzheimer’s disease. While we’re not emphasizing that disease indication, it’s certainly something we’re looking at in the lab.
Liver disease, particularly for things like non-alcoholic fatty liver, is something that we think has a lot of potential as well. So, we’re working on all aspects of the impact of oxidized cholesterol.
We also have this basic technology that is built to sequester things that are small and toxic that accumulate in biological systems. We could potentially use that as a detoxifier of things that accumulate with age. There’s other things that we’re interested in, like bisretinoids that accumulate in the eye in macular degeneration that we’re looking closely at.
We are also working on finding solutions to nanoplastics, things like BPA and PFAS that we think our technology could potentially address. Firstly, at a therapeutic level, in people who’ve accumulated unhealthy levels of nanoplastics that we could clean out of the blood, cells and tissues where they’re building up.
Secondly, environmental remediation is another possible area of interest. You could create something with our technology that’s very specific and potent for removing it from the environment. So, you might use it to remove nanoplastics and other pollution from the soil or water. Obviously, environmental remediation isn’t our focus. We’re a biomedical company, but we’re looking at collaborating with organizations that want to use our technology for other things unrelated to what we’re working on such as environmental remediation.
Well, if this succeeds, I think you folks deserve the Nobel Prize.
Thank you, Steve, but we’re not in it for the prizes or accolades, we’re in it to have a massive impact on humanity for the better. What I’d like to say to my team is that we could make a billion dollars and it’s not just a billion-dollar industry, it’s a trillion-dollar industry. But it’s not about making a billion dollars or a trillion dollars. It’s about saving a billion lives. And that’s when we’ll be true billionaires. The first true billionaire will be the person or the team who has saved a billion lives. And that’s the kind of billionaire that I want to become.